Remember those soaring profits that propelled the stocks of health insurers to record highs starting in 2013?
Like how UnitedHealth Group Inc. (NYSE: UNH) hit an all-time high in June 2013 and never looked back? From January 2013 to January 2016, UNH stock nearly tripled the performance of the Standard & Poor's 500 Index.
Humana Inc. (NYSE: HUM) fared even better, hitting an all-time high in September 2013. In that same three-year period HUM stock more than quadrupled the gains in the S&P 500.
Turns out those same health insurers fattened their profits with a lot of help from a years-long strategy to defraud the Medicare Advantage program.
And since Medicare derives its funding from the government, these health insurers have essentially been stealing money from you, the U.S. taxpayer, for their own gain.
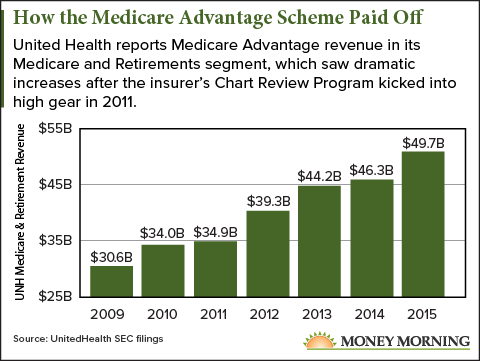
And gain they did, to the tune of billions ...
"There Was No Way They Could Lose"
The poster child for this scheme is UnitedHealth Group, the nation's largest insurer. And as the biggest provider of "Medicare Advantage" plans (nearly 4 million enrollees as of December 2016), UnitedHealth stood to benefit the most.
According to a U.S. Department of Justice lawsuit filed May 16, between 2010 and 2015 UnitedHealth siphoned off about $3 billion in taxpayer money by overbilling Medicare Advantage. But the pattern of overpayments dates back as far as 2006.
"As the nation's largest Medicare Advantage organization, UHG received substantial overpayments based upon untruthful and inaccurate information about the health status of those enrolled in its plans," said Acting U.S. Attorney for the Western District of New York James P. Kennedy Jr. in a Justice Department statement. "Such fraudulent spending of taxpayers' dollars will not be tolerated."
The suit is based on the allegations of whistleblower Benjamin Poehling, a former finance director for UnitedHealth who worked there from 2002 to 2012.
"They've set up a perfect scheme here," Poehling told The New York Times. "It was rigged so there was no way they could lose."
UnitedHealth disputes any wrongdoing. A UNH spokesman told the Times that his company "complied with the government's Medicare Advantage program rules," while criticizing the policies of the Centers for Medicare and Medicaid Services (CMS) as "murky."
Don't Miss: Start Collecting a "Second Salary" with These Powerful Income Generators
UnitedHealth is the only insurer named in the suit, but the Justice Department is investigating several other leading insurers for the same kind of Medicare Advantage fraud.
A prior complaint, filed in 2011, listed Aetna Inc. (NYSE: AET) and Humana Inc. as defendants. Humana has the second-highest number of Medicare Advantage enrollees, 3.21 million.
Other health insurers could be caught in the Justice Department's web through acquisitions of companies named in the 2011 complaint: Centene Corp. (NYSE: CNC) via its 2016 merger with HealthNet, and Cigna Corp. (NYSE: CI) through its 2011 acquisition of Bravo Health-parent HealthSpring.
That so many health insurance companies have come under scrutiny speaks to how easy it was to cheat the Medicare Advantage program - and steal more money out of taxpayer pockets.
Here's what the insurers were doing...
How the Health Insurers Poached Your Tax Dollars
When Medicare Advantage was created 14 years ago, it made private health insurers like UnitedHealth middlemen between beneficiaries and the government.
Under Medicare Advantage, the government reimburses insurers a base rate for each member it enrolls. But certain medical conditions, or combinations of medical conditions, can increase the reimbursements. The idea was to prevent the insurers from targeting only the healthiest (and thus most profitable) prospects.
But the idea backfired. Paying extra for a variety of conditions created an incentive to exaggerate a member's health problems to increase reimbursement rates.
Take, for example, a typical male beneficiary between the ages of 70 and 74. The base payment to an insurer for such a patient in Medicare Advantage is $3,866 per year. But tacking on health conditions can inflate the annual payment to multiples of that amount.
Obviously, many of the diagnoses given in the last 10 years were legitimate. But the insurers could game the system in subtle ways. A diagnosis of diabetes without complications adds $1,058 to the annual payment. But diabetes with complications adds triple that amount - $3,251.
The trick was finding the patients with conditions conducive to this scheme. And technology had the answer in Big Data.
The insurers used complex data-mining programs to identify patients with conditions that could be "enhanced" without raising government suspicion.
Staff would then examine the medical records in a process called "risk scoring," in what amounted to a treasure hunt for profits at the government's expense.
If the process happened to show that a patient had an unsupported diagnosis, UNH was obligated to delete it. But since that would mean less money for UnitedHealth, the company disregarded such information.
The potential of this process - the so-called "chart review program" - to fatten the company's bottom line quickly became apparent...
"Let's Turn on the Gas!"
[mmpazkzone name="in-story" network="9794" site="307044" id="137008" type="4"]
UnitedHealth increased its efforts to sign up more Medicare Advantage customers while simultaneously increasing the number of patient records it reviewed each year.
From 2007 to 2015, UnitedHealth more than doubled its number of Medicare Advantage patients.
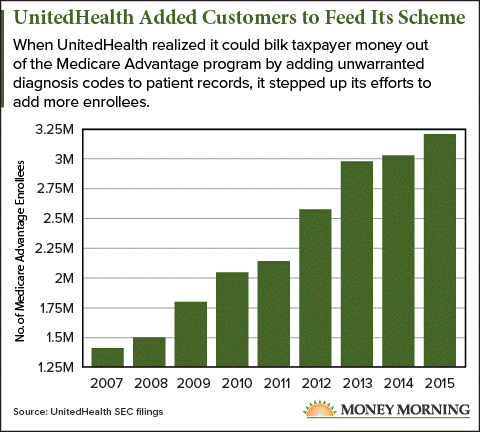
According to the Justice Department lawsuit, UnitedHealth reviewed 600,000 charts in 2006. The resulting "condition inflation" of added diagnosis codes produced $270 million in extra revenue.
By 2011, UNH was reviewing 1.5 million charts per year, increasing their reward to $426 million.
According to the Justice Department, the rapid increase in chart reviews was part of a concerted effort by management to squeeze more money out of the Medicare Advantage program.
The original complaint includes a memo from the chief financial officer of UnitedHealth's Medicare & Retirement division, Jerry Knutson, to Jeff Dumcum of Ingenix, the UNH subsidiary doing the data screening that lays bare the company's motives.
"Wanted to get together with you and discuss what we can do in the short term and long term to really go after the potential risk scoring you have consistently indicated is out there," Knutson wrote in the Nov. 7, 2007, memo. "You mentioned vasculatory disease opportunities, screening opportunities, etc. with huge $ opportunities. Let's turn on the gas!"
Knutson continues: "When we meet next on our steering committee, I'd like to see what it would take to add another $100M to our 2008 revenue from where we are. What would be doable? What resources would you need? What technology would you need?"
This annual revenue bonus from these efforts continued to grow as UnitedHealth perfected its chart review program, reaching $882 million by 2014.
Meanwhile, UNH stock was going on a tear...
UnitedHealth Stock Soars on Ill-Gotten Revenue
UnitedHealth stock has soared more than 450% since Jan. 1, 2010, nearly quadrupling the 117% gain of the Standard & Poor's 500 index.
Over the last three years, with the chart review program in full gear, UNH stock has done even better, with gains of 128% - more than quadrupling the S&P 500's 27.5% increase.
And keep in mind these massive gains have come despite cumulative losses of about $1 billion from the Obamacare exchanges over the past two years.
The question now is whether the government will prevail against UnitedHealth, and if so, what kind of penalty it can exact. The suit asks for triple damages and penalties but not a specific sum.
The stakes for this case are particularly high. How the UnitedHealth suit fares may well determine how the government will proceed against the health insurers named in the 2011 complaint.
But the government also might want to rethink its Medicare Advantage policies.
"CMS could do a lot to change the rules so it's not so easy to get away with this stuff," Timothy Layton, an assistant professor at Harvard Medical School who focuses on health insurers, told The New York Times. "What the insurers are doing is not socially valuable at all."
Must See: What do billionaires Peter Lynch, President Trump, and a retired cop from Northridge have in common? They've all benefitted enormously from a curious Great Depression-era "program." And even though most have no idea this exists, it could be worth $68,870 or more to the average American. Continue reading...
Follow me on Twitter @DavidGZeiler and Money Morning on Twitter @moneymorning, Facebook, or LinkedIn.
Related Articles:
- The New York Times: A Whistle-Blower Tells of Health Insurers Bilking Medicare
About the Author
David Zeiler, Associate Editor for Money Morning at Money Map Press, has been a journalist for more than 35 years, including 18 spent at The Baltimore Sun. He has worked as a writer, editor, and page designer at different times in his career. He's interviewed a number of well-known personalities - ranging from punk rock icon Joey Ramone to Apple Inc. co-founder Steve Wozniak.
Over the course of his journalistic career, Dave has covered many diverse subjects. Since arriving at Money Morning in 2011, he has focused primarily on technology. He's an expert on both Apple and cryptocurrencies. He started writing about Apple for The Sun in the mid-1990s, and had an Apple blog on The Sun's web site from 2007-2009. Dave's been writing about Bitcoin since 2011 - long before most people had even heard of it. He even mined it for a short time.
Dave has a BA in English and Mass Communications from Loyola University Maryland.



